|
|
Title:
Author:
Date Posted:
Source:
|
HEADACHE IN CHILDREN AND ADOLESCENTS
September 2010
|
Introduction
Headache is a common complaint among children and adolescents. The prevalence of headache varies by age and gender through out childhood and adolescence. Migraine begins earlier in boys than in girls. Until the age of seven, the prevalence of migraine in boys is slightly more than in girls. By menarche, the prevalence of migraine in boys and girls is roughly equal. However, after menarche, the prevalence of migraine begins to be more predominant in girls. This separation based on gender increases even further in late adolescence (15-19 years of age) when 28% of girls and 14% of boys are affected by migraine. Headaches, especially migraines, significantly impact the lives of children and adolescents. Approximately 65-80% of children with migraine headaches experience disruption of their normal daily activities at home, school, and social settings. The burden of migraine may also result in the development of emotional changes such as anxiety or sadness. Such disruptions create significant disability and affect the quality of the childís life. Thus, early recognition and management of headaches in children and adolescents can significantly improve quality of life in the short and long terms.
Headache disorders can be categorized as either primary or secondary. As with adults, the vast majority of headaches in children and adolescents are primary headache disorders, especially migraine (with or without aura), tension-type headache, and chronic daily headache. Secondary headache disorders, although much less common, can be due to various organic etiologies which can range from the relatively benign to the seriously life-threatening including acute febrile illness, rhinosinusitis, dental abscess, hypertension, diabetic ketoacidosis, intracranial and extracranial infections, head or neck trauma, vascular malformations, subarachnoid hemorrhage, intracranial mass lesions, etc.
Diagnostic Approach
The overwhelming majority of headache disorders can be diagnosed by a thorough history and physical examination. Although headache can be a presenting symptom of underlying organic pathology, gathering accurate data from the patient and patientís family is often enough to identify or rule out serious etiologies. However, doing so can be exceedingly difficult because patients and their parents often attribute headaches and nausea to "the flu" or dismiss them as "sinus headaches." Careful attention must be paid to obtaining the patientís description of headache onset, timing, frequency, duration, severity, quality/character, location, precipitating factors/triggers, associated symptoms (especially nausea/vomiting, photophobia, phonophobia) and any aggravating and/or alleviating factors. Of course, a thorough past medical history, family history, medication history (including prescription, over-the-counters, and vitamins/herbs), allergy history, previous diagnostic workup, previous treatment history (pharmacological and non-pharmacological) and social history should also be obtained in order to assist the clinician with identifying potential underlying etiologies, comorbidities, and the impact of headache on the patient and the patientís family.
In adults, the mnemonic "SNOOP" is commonly used to represent diagnostic red flags of potentially worrisome secondary causes of headache. An application of the "SNOOP" mnemonic to the pediatric population can be made by omitting the second "O" which denotes new onset headache in those over 50 years of age. In doing so, "SNOOP" can be reorganized into "PONS" as follows:
- Previous headache history or headache progression (change in attack character, frequency, or clinical features)
- Onset (sudden, abrupt, split-second)
- Neurologic symptoms and/or abnormal/focal signs (ataxia, seizures, mental status changes such as confusion, impaired alertness and/or consciousness)
- Systemic symptoms (fever, weight loss) or Secondary headache risk factors (systemic cancer, HIV, rheumatologic/connective tissue disorders)
Other potential indicators of organic pathology can include headache which awakens a child from sleep, severe vomiting, and the absence of a family history of migraine. If any of these red flags are discovered upon a thorough history and physical examination, the appropriate laboratory and/or imaging investigations should be performed.
If a primary headache disorder is highly suspected, further laboratory investigation is usually not warranted. However, laboratory investigations can be obtained to serve as baseline values for periodic monitoring of potential medication adverse effects. These baseline labs usually include but are not limited to a complete blood count with differential, comprehensive metabolic panel, and a lipid panel.
Neuroimaging studies are usually not indicated in children with a history consistent with a primary headache disorder (especially migraine or tension-type) and a normal neurologic examination. Such children will not usually have significantly abnormal findings on head CT scans or intracranial MRIs. A small percentage may have incidental and/or unrelated findings, but routine neuroimaging is not indicated in children with primary headaches.
Electroencephalography (EEG) is usually not indicated in the routine diagnostic assessment of pediatric headache patients. An EEG should be performed on patients with an atypical migraine aura, episodic loss of consciousness, or symptoms suggestive of a seizure disorder. Background slowing may be appreciated during some migraine attacks, but the EEG results are usually normal.
Lumbar puncture (LP) is indicated if meningitis, encephalitis, subarachnoid hemorrhage, or high-low pressure syndromes are suspected. Cerebrospinal fluid studies and pressure measurement should be also be performed, especially if the history and/or physical examination are not consistent with migraine headache. In those patients where increased intracranial pressure is suspected or in those with focal neurologic deficits, a head CT scan or similar neurologic imaging modality should be performed prior to a lumbar puncture. However, if meningitis or encephalitis is highly suspected in a toxic appearing patient, treatment should not be delayed in order to perform the head CT scan and LP first.
Once a secondary headache disorder is sufficiently ruled out, an accurate diagnosis of a primary headache disorder can be made according to the criteria set forth in the International Classification of Headache Disorders — 2nd revision (ICHD-II). Although some deficiencies remain in this most current revision of the ICHD for the diagnosis of migraine in children, the criteria for migraine in adults contain footnotes which make special allowances for the differential presentation of migraine in children. These footnotes serve to broaden the scope of the criteria and improve diagnostic ability. The use of these criteria helps to bring uniformity to the diagnosis of migraine in children and to improve diagnostic expertise and confidence. This article assumes that the reader possesses the basic understanding and knowledge to make a diagnosis of migraine in children. For more information regarding the diagnosis of other primary headache disorders, please refer to the ICHD-II.
Biopsychosocial Approach to Management
The pervasive nature of headaches and related comorbidities in the lives of children, adolescents, and their families requires a comprehensive biopsychosocial approach. Such an approach necessitates the multidisciplinary collaboration of various medical and behavioral specialists working together to improve a patientís overall functioning and quality of life. The combination of both pharmacologic and non-pharmacologic treatments provides a significant advantage over using either modality alone. Non-pharmacologic treatments are especially important as they are typically more effective in children and help to minimize medications as much is possible.
Non-Pharmacologic Treatments
Non-pharmacologic modalities of treatment generally consist of patient education, lifestyle strategies, and behavioral interventions. Patient education should be the first step taken once a diagnosis has been made. A detailed explanation of the diagnosis and the legitimization of the headache as a physiological disorder are of primary importance. Beyond these aspects of their headaches, children and their parents usually want to hear three things from the physician: (1) the cause of the headache (including triggers), (2) treatment and prognosis, and (3) reassurance that a primary headache disorder is not serious. It is also important that realistic goals and expectations are set during this phase of treatment. Children and their parents should understand that there are no "miracle cures" for headaches. As such, they should be encouraged to take an active role in the management of their headaches, which non-pharmacologic techniques offer.
At this point, it is usually helpful to introduce the use of a headache diary as a means to identify specific triggers of the patientís headaches so that patients can take steps to avoid potentially aggravating factors. Of course, some triggers (e.g. weather changes, stress, hormonal influences) cannot be avoided, but certainly many (e.g. missing meals, bright lights/sunlight, undersleeping/oversleeping, certain foods, perfume, cigarette smoke, physical exertion) can be. Headache diaries are also helpful as a means to record the frequency and severity of headaches as well as document treatment efficacies and side effects. Another major advantage of using a headache diary is that it improves the accuracy of a patientís recall of their headaches between office visits with the physician.
Lifestyle strategies should include discussion of the importance of proper diet, exercise, and sleep hygiene. Headache patients, in general, do better with regular schedules, eating three or more meals per day, and going to bed and awakening at the same time every day including weekends. Daily exercise can be particularly helpful for headache patients. Patients should strive to get at least 30 minutes of exercise per day. Generally, headache patients do better with low impact exercises such as swimming, walking, biking, and yoga. Of course, if physical exertion is a significant trigger for a patient, rigorous and/or high impact exercise should be minimized or avoided unless the exertionally triggered headaches can be prevented with medication.
Behavioral interventions such as psychotherapy/counseling and relaxation techniques can be particularly helpful for patients who experience significant stress in their lives. Children and adolescents may be involved in too many activities and feel extremely overwhelmed. The incidence of hard driving perfectionistic behavior and depression is increased in adolescents with severe headache. Children and adolescents may miss substantial blocks of time in school and/or social activities. Such patients need to be assessed for depression, school phobia, and secondary gains. Peer groups or individual counseling for children as well as family centered therapy for children and their parents are often helpful and an indispensable augmentation to medical therapy.
Relaxation techniques such as biofeedback, deep breathing, and imaging should be encouraged in children and adolescents with frequent headaches. Most children and adolescents can often learn relaxation techniques from books or audiovisual aids that are readily available in bookstores, so that extended visits to a therapist to learn relaxation techniques are not required. However, if patients are willing and able to see a therapist, seeing a therapist who teaches biofeedback can be very useful. Most children under the age of 9 cannot learn and apply biofeedback, but some 7 or 8 year olds can learn simple breathing and imaging techniques that may help their headaches.
Pharmacologic Treatment
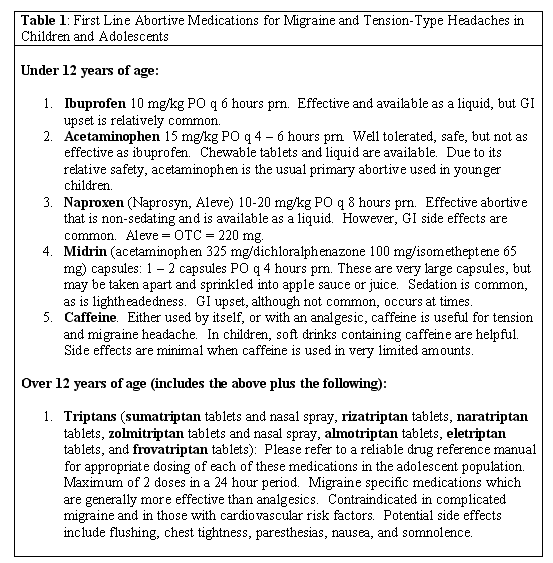
There are two major types of pharmacologic treatment for headaches: abortive and preventive. The decision as to how much medication to use depends upon the frequency and severity of the headaches and how much they bother the child or adolescent. Some children are simply not bothered by their daily headaches and tend to simply ignore them. Others may be incapacitated and miss an entire year of school. As with adult headaches, in children and adolescents, abortive medication is used in the overwhelming majority of cases, without daily preventive medication. Before being prescribed abortive medications, patients and their parents need to be instructed in the proper use of the abortive in order to optimize its efficacy. Patients should be instructed to use their abortive medication while their headaches are mild. Waiting to "see how bad it will get" before taking the abortive renders it less effective. See Table 1 for a list of first line abortive medications for migraine and tension-type headache in children and adolescents.
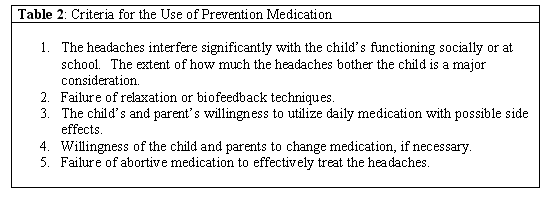
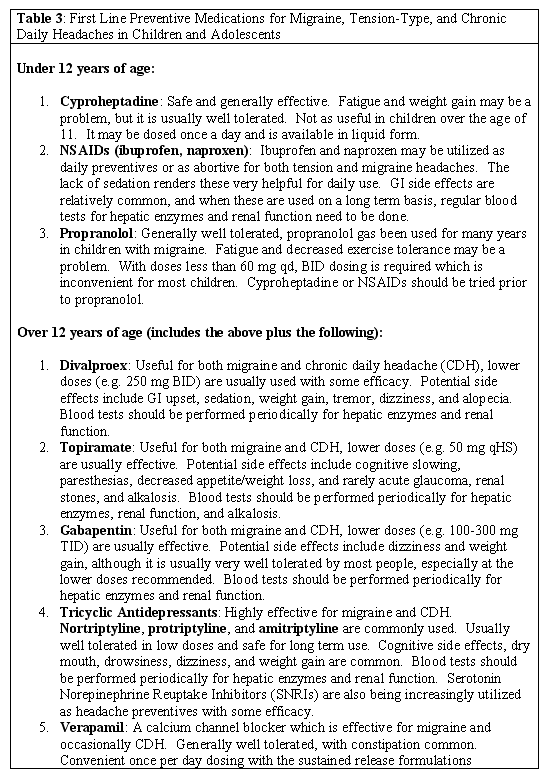
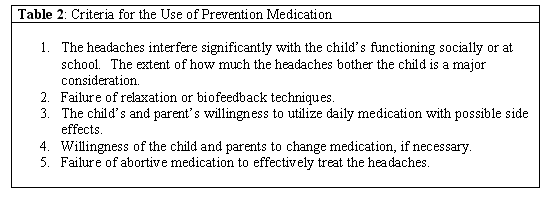
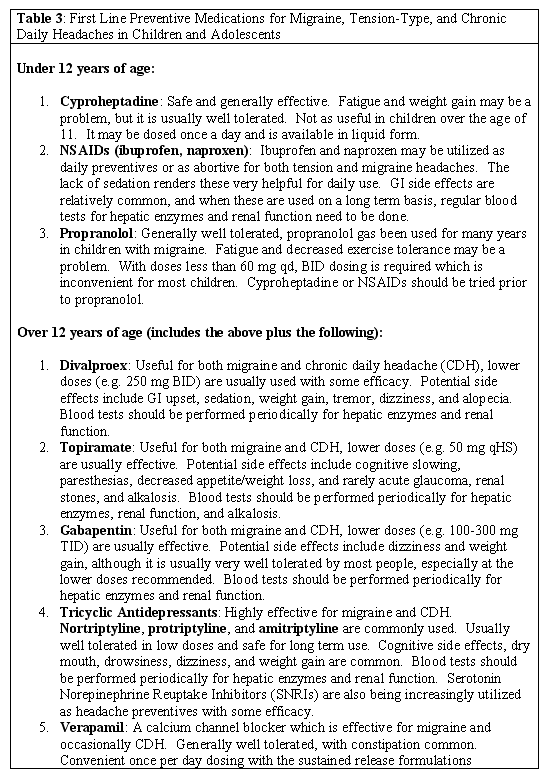
With frequent migraines that are more than mild, or for moderate to severe daily headaches, daily preventive medication may be necessary. In order to minimize medications and their potential adverse effects, it is usually wise to start at a low dose of a daily preventive and slowly titrate up to reasonable efficacy. See Table 2 for a more complete list of criteria for the use of preventive medication in children and adolescents. It is always reasonable to try biofeedback as the first step, with simple abortive medications, and attempt to avoid daily preventive medication if possible. See Table 3 for a list of first line preventive medications for migraine and tension-type headache in children and adolescents.
Realistic goals and expectations for both abortive and preventive medications should be discussed with the patient and patientís family. For abortive medications, the goal is to achieve significant headache and associated symptom relief (>70%) in 2 hours. When preventive medications are used, the goal is to reduce headache frequency and severity by 30% - 50% and/or to improve headache related disability. Sometimes, patients will also note that the efficacy of their abortive medications improves with the use of a daily preventive.
When preventive medications are used in children and adolescents, it is prudent to periodically (approximately every 3 to 6 months) attempt to discontinue the daily preventive in an effort to minimize medications. As with adults, the idea is to see if the patient may return to simply using abortive medication. However, if an adolescent has had headaches for a number of years, it is best to not be so quick to discontinue a successful preventive.
Conclusion
Once a comprehensive multidisciplinary management plan has been put into place, regular follow up with the patient and ongoing collaboration with other involved health car professionals is essential. Management of headache disorders in children and adolescents is a trial and error process. There is no "cookie cutter" approach. Vigilance and patience are required in order to achieve any success. In the long term, it helps to not overly focus on the quantitative variables such as frequency and severity. Although frequency and severity of headaches are important, success is ultimately measured by how much we can help a child to return to more normal home, school, and social functioning so that they have a better overall quality of life. After all, health is much more than just the absence of disease; it encompasses a sense of well-being that empowers.
|